Dive Brief:
- Anthem Inc. is setting up its own drug plan, a sign that the insurer may be breaking with Express Scripts Holding Co., a pharmacy-benefits management (PBM) firm, Bloomberg reports. The split comes after Anthem accused the St. Louis-based PBM of overcharging it by $3 billion dollars.
- The change gives Anthem more ammunition in its competition against rival UnitedHealth Group Inc. according to Bloomberg. UnitedHealth also owns a PBM, OptumRx, which brought the largest insurer in the U.S. $16 billion in revenues in Q3 2017, says Bloomberg.
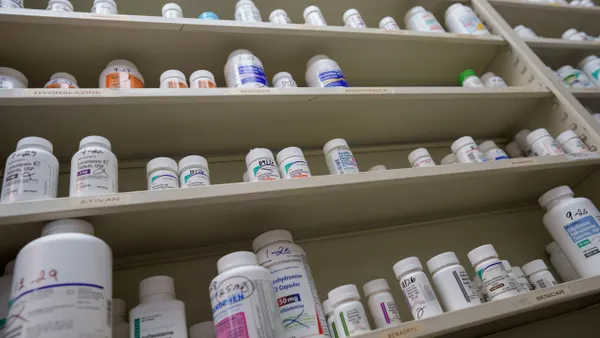
- PBMs administer complicated drug contracts and negotiate prices as a middleman. These business units have also come under scrutiny by Washington lawmakers. Pharma manufacturers blame PBMs for driving up prescription drug costs.
Dive Insight:
This is Anthem's biggest structural announcement since the failure of a high-profile merger with Cigna back in February. A federal judge struck the agreement down in part because it was deemed non-competitive.
Now the focus has pivoted to what could prove to be a consequential trend for big pharma: Will insurance companies eschew PBMs to set up their own drug plans to hold prescription drug costs down or are PBMs high profit-making business units? And will employers be able to negotiate the best prices for their healthcare plans? These questions need answers, as employers find ways to keep prescription-drug costs and healthcare costs low in general.
An Aon study predicts a 7.2% increase in healthcare cost next year. The National Business Group on Health puts the increase for healthcare and drug costs at 5%, and many in the benefits industry point fingers at PBMs and the secrecy with which they formulate manufacturer contracts as a reason for the hikes. Considering the expense of employee benefits, employers won't be able to sit on the sidelines of this debate.
Treatment for the opioid addiction epidemic could push up drug prices, too, even with federal government subsidies. It should be noted that at least one PBM, CVS Caremark, has pledged to take measures to combat the epidemic.